Where Art meets Science to create Beautiful Smile
- TEXT US: 8608798999
- MenuMenuMenuMenu
Where Art meets Science to create Beautiful Smile
Where Art meets Science to create Beautiful Smile
Menu
- MenuMenuMenuMenu
Where Art meets Science to create Beautiful Smile
Where Art meets Science to create Beautiful Smile
Pulling a Tooth (Tooth Extraction)
Having a tooth pulled in adulthood is sometimes necessary.
Reasons for Pulling Teeth
Although permanent teeth were meant to last a lifetime, there are several reasons why tooth extraction may be needed. A widespread basis involves a tooth that is too badly damaged, from trauma or decay, to be repaired. Other reasons include:
A crowded mouth. Sometimes dentists pull teeth to prepare the mouth for orthodontia. The goal of orthodontia is to properly align the teeth, which may not be possible if your teeth are too big for your mouth. Likewise, if a tooth cannot break through the gum (erupt) because there is no room in the mouth for it, your dentist may recommend pulling it.
Infection. If tooth decay or damage extends to the pulp — the center of the tooth containing nerves and blood vessels — bacteria in the mouth can enter the pulp, leading to infection. Often this can be corrected with root canal therapy (RCT), but if the disease is so severe that antibiotics or RCT do not cure it, extraction may be needed to prevent the spread of infection.
Risk of infection. If your immune system is compromised (for example, if you are receiving chemotherapy or have an organ transplant), even the risk of infection in a particular tooth may be enough to pull the tooth.
Periodontal (gum) disease. If periodontal disease — an infection of the tissues and bones that surround and support the teeth — has caused the teeth to loosen, it may be necessary to pull the tooth or teeth.
What to Expect With Tooth Extraction
Dentists and oral surgery (dentists with special training to perform surgery) perform tooth extractions. Before pulling the tooth, your dentist will give you an injection of a local anesthetic to numb the area where the tooth will be removed.
If the tooth is impacted, the dentist will cut away gum and bone tissue that cover the tooth and then, using forceps, grasp the tooth and gently rock it back and forth to loosen it from the jaw bone and ligaments that hold it in place. Sometimes, a hard-to-pull tooth must be removed in pieces.
Once the tooth has been pulled, a blood clot usually forms in the socket. The dentist will pack a gauze pad into the socket and have you bite down on it to help stop the bleeding. Sometimes the dentist will place a few stitches — usually self-dissolving — to close the gum edges over the extraction site.
Sometimes, the blood clot in the socket breaks loose, exposing the bone in the socket. This is a painful condition called dry socket. If this happens, your dentist will likely place a sedative dressing over the socket for a few days to protect it as a new clot form.





Pulling a Tooth (Tooth Extraction)
Having a tooth pulled in adulthood is sometimes necessary.
Reasons for Pulling Teeth
Although permanent teeth were meant to last a lifetime, there are several reasons why tooth extraction may be needed. A widespread basis involves a tooth that is too badly damaged, from trauma or decay, to be repaired. Other reasons include:
A crowded mouth. Sometimes dentists pull teeth to prepare the mouth for orthodontia. The goal of orthodontia is to properly align the teeth, which may not be possible if your teeth are too big for your mouth. Likewise, if a tooth cannot break through the gum (erupt) because there is no room in the mouth for it, your dentist may recommend pulling it.
Infection. If tooth decay or damage extends to the pulp — the center of the tooth containing nerves and blood vessels — bacteria in the mouth can enter the pulp, leading to infection. Often this can be corrected with root canal therapy (RCT), but if the disease is so severe that antibiotics or RCT do not cure it, extraction may be needed to prevent the spread of infection.
Risk of infection. If your immune system is compromised (for example, if you are receiving chemotherapy or have an organ transplant), even the risk of infection in a particular tooth may be enough to pull the tooth.
Periodontal (gum) disease. If periodontal disease — an infection of the tissues and bones that surround and support the teeth — has caused the teeth to loosen, it may be necessary to pull the tooth or teeth.

What to Expect With Tooth Extraction
Dentists and oral surgery (dentists with special training to perform surgery) perform tooth extractions. Before pulling the tooth, your dentist will give you an injection of a local anesthetic to numb the area where the tooth will be removed.
If the tooth is impacted, the dentist will cut away gum and bone tissue that cover the tooth and then, using forceps, grasp the tooth and gently rock it back and forth to loosen it from the jaw bone and ligaments that hold it in place. Sometimes, a hard-to-pull tooth must be removed in pieces.
Once the tooth has been pulled, a blood clot usually forms in the socket. The dentist will pack a gauze pad into the socket and have you bite down on it to help stop the bleeding. Sometimes the dentist will place a few stitches — usually self-dissolving — to close the gum edges over the extraction site.
Sometimes, the blood clot in the socket breaks loose, exposing the bone in the socket. This is a painful condition called dry socket. If this happens, your dentist will likely place a sedative dressing over the socket for a few days to protect it as a new clot form.

What to Tell Your Dentist before You Have a Tooth Pulled
Although having a tooth pulled is usually very safe, the procedure can allow harmful bacteria into the bloodstream. Gum tissue is also at risk of infection. If you have a condition that puts you at high risk for developing a severe infection, you may need to take antibiotics before and after the extraction. Before having a tooth pulled, let your dentist know your complete medical history, the medications, and supplements you take, and if you have one of the following (note that this list is not complete):
– Damaged or man-made heart valves
– Congenital heart defect
– Impaired immune system
– Liver disease (cirrhosis)
– Artificial joint, such as a hip replacement
– History of bacterial endocarditis
After You’ve Had a Tooth Pulled
Following an extraction, your dentist will send you home to recover. Recovery typically takes a few days. The following can help minimize discomfort, reduce the risk of infection, and speed recovery.
– Take painkillers as prescribed.
– Bite firmly but gently on the gauze pad placed by your dentist to reduce bleeding and allow a clot to form in the tooth socket. Change gauze pads before they become soaked with blood. Otherwise, leave the pad in place for three to four hours after the extraction.
– Apply an ice bag to the affected area immediately after the procedure to keep swelling. Apply ice for 10 minutes at a time.
– Relax for at least 24 hours after the extraction, and limit activity for the next day or two.
– Avoid rinsing or spitting forcefully for 24 hours after the extraction to avoid dislodging the clot that forms in the socket.
– After 24 hours, rinse with your mouth with a solution made of 1/2 teaspoon salt and 8 ounces of warm water.
– Do not drink from a straw for the first 24 hours.
– Do not smoke, which can inhibit healing.
– Eat soft foods, such as soup, pudding, yogurt, or applesauce, the day after the extraction. Gradually add solid foods to your diet as the extraction site heals.
– When lying down, prop your head with pillows. Lying flat may prolong bleeding.
– Continue to brush and floss your teeth, and brush your tongue, but be sure to avoid the extraction site. Doing so will help prevent infection.
When to Call the Dentist
It is normal to feel some pain after the anesthesia wears off. For 24 hours after having a tooth pulled, you should expect some swelling and residual bleeding. However, if either bleeding or pain is still severe more than four hours after your tooth is pulled, you should call your dentist. You should also contact your dentist if you experience any of the following:
– Signs of infection, including fever and chills
– Nausea or vomiting
– Redness, swelling, or excessive discharge from the affected area
– Cough, shortness of breath, chest pain, or severe nausea or vomiting
The initial healing usually takes about one to two weeks, and new bone and gum tissue will grow into the gap. Over time, however, having a tooth (or teeth) missing can cause the remaining teeth to shift, affecting your bite and making it difficult to chew. For that reason, your dentist may advise replacing the missing tooth or teeth with an implant, fixed bridge, or denture.
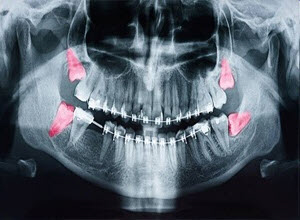
Wisdom Teeth Extractions
Wisdom teeth, or third molars, do not always erupt properly when they decide to make an appearance. It’s wise to get an early opinion from your dentist on getting wisdom teeth pulled before they become impacted, causing pain, swelling, infection, cavities, or gum disease.
Why don’t wisdom teeth grow in the right?
Although we have seen a reduction in the size of the human jaw during human evolution, we still retain the same number of teeth. The change in jaw size of modern humans is related to the discovery and use of fire to prepare food, and the development of crude tools, such as blades, to process food. These advances enhanced the culinary skills and diet of early humans; they significantly lightened the workload of the jaw. The result? As the need for a powerful jaw vanished, the jaw became smaller, the teeth became crowded, and the space required for the proper growth of wisdom teeth was no longer available. (The modern human mouth is too small to accommodate wisdom teeth, which make their appearance in young adults between 15-25.)
What does “impacted” mean?
When wisdom teeth don’t have room to grow or haven’t reached their final position by age 25, they are considered impacted- no place to go and no plans to expand. Third molar impaction is the most prevalent medical, developmental disorder. A complete set of healthy teeth sometimes doesn’t leave much room for wisdom teeth to erupt.
What kind of problems can impact third molars cause?
Partially erupted wisdom teeth are breeding grounds for bacteria and germs and may lead to infection. In addition to jaw pain and gum disease, which may also develop, impacted third molars are mature sites for the growth of tumors and cysts. Not all wisdom teeth cause problems, however.

Can’t I use an antibiotic?
Antibiotics only soothe infected wisdom teeth for a short time. Since people frequently use a wide variety of antibiotics, the infection may be resistant to such medication and doesn’t solve the real problem: The tooth can’t fit in your mouth.
When is removal necessary?
It isn’t wise to wait until wisdom teeth bother you. As advised by your dentist, early removal is generally recommended to avoid problems, such as an impacted tooth that destroys the second molar. People younger than 16 heal easier too. At an early age, people should be evaluated by their dentist, who can track third molar development with the help of X-rays. Second, molars should be visible to lessen damaging them during surgery. This occurs at age 11 or 12, so wisdom teeth should be removed when the decision has been made that they cannot erupt into a good position.
What if I don’t have any symptoms?
People with symptoms of impaction, such as pain, swelling, and infection, should have their wisdom teeth removed immediately. However, those with no symptoms can avoid the chance of ever suffering from the pain of impacted wisdom teeth or achieve better orthodontic treatment results by having them removed. Symptomatic impacted wisdom teeth also should be removed to reduce the chance of unexplained pain, accommodate prosthetic appliances, or avoid cavities, periodontal disease, bone shrinkage, and tumor development.
How is the tooth removed?
Surgery for impacted wisdom teeth involves:
What is tooth extraction cost?
If you are searching for affordable tooth extraction near me than visiting Smile Ora Dental is the best choice.
What to Tell Your Dentist before You Have a Tooth Pulled
Although having a tooth pulled is usually very safe, the procedure can allow harmful bacteria into the bloodstream. Gum tissue is also at risk of infection. If you have a condition that puts you at high risk for developing a severe infection, you may need to take antibiotics before and after the extraction. Before having a tooth pulled, let your dentist know your complete medical history, the medications, and supplements you take, and if you have one of the following (note that this list is not complete):
– Damaged or man-made heart valves
– Congenital heart defect
– Impaired immune system
– Liver disease (cirrhosis)
– Artificial joint, such as a hip replacement
– History of bacterial endocarditis
After You’ve Had a Tooth Pulled
Following an extraction, your dentist will send you home to recover. Recovery typically takes a few days. The following can help minimize discomfort, reduce the risk of infection, and speed recovery.
– Take painkillers as prescribed.
– Bite firmly but gently on the gauze pad placed by your dentist to reduce bleeding and allow a clot to form in the tooth socket. Change gauze pads before they become soaked with blood. Otherwise, leave the pad in place for three to four hours after the extraction.
– Apply an ice bag to the affected area immediately after the procedure to keep swelling. Apply ice for 10 minutes at a time.
– Relax for at least 24 hours after the extraction, and limit activity for the next day or two.
– Avoid rinsing or spitting forcefully for 24 hours after the extraction to avoid dislodging the clot that forms in the socket.
– After 24 hours, rinse with your mouth with a solution made of 1/2 teaspoon salt and 8 ounces of warm water.
– Do not drink from a straw for the first 24 hours.
– Do not smoke, which can inhibit healing.
– Eat soft foods, such as soup, pudding, yogurt, or applesauce, the day after the extraction. Gradually add solid foods to your diet as the extraction site heals.
– When lying down, prop your head with pillows. Lying flat may prolong bleeding.
– Continue to brush and floss your teeth, and brush your tongue, but be sure to avoid the extraction site. Doing so will help prevent infection.
When to Call the Dentist
It is normal to feel some pain after the anesthesia wears off. For 24 hours after having a tooth pulled, you should expect some swelling and residual bleeding. However, if either bleeding or pain is still severe more than four hours after your tooth is pulled, you should call your dentist. You should also contact your dentist if you experience any of the following:
– Signs of infection, including fever and chills
– Nausea or vomiting
– Redness, swelling, or excessive discharge from the affected area
– Cough, shortness of breath, chest pain, or severe nausea or vomiting
The initial healing usually takes about one to two weeks, and new bone and gum tissue will grow into the gap. Over time, however, having a tooth (or teeth) missing can cause the remaining teeth to shift, affecting your bite and making it difficult to chew. For that reason, your dentist may advise replacing the missing tooth or teeth with an implant, fixed bridge, or denture.
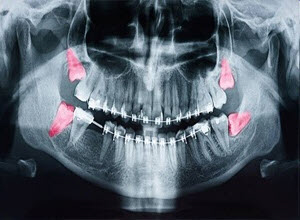
Wisdom Teeth Extractions
Wisdom teeth, or third molars, do not always erupt properly when they decide to make an appearance. It’s wise to get an early opinion from your dentist on getting wisdom teeth pulled before they become impacted, causing pain, swelling, infection, cavities, or gum disease.
Why don’t wisdom teeth grow in the right?
Although we have seen a reduction in the size of the human jaw during human evolution, we still retain the same number of teeth. The change in jaw size of modern humans is related to the discovery and use of fire to prepare food, and the development of crude tools, such as blades, to process food. These advances enhanced the culinary skills and diet of early humans; they significantly lightened the workload of the jaw. The result? As the need for a powerful jaw vanished, the jaw became smaller, the teeth became crowded, and the space required for the proper growth of wisdom teeth was no longer available. (The modern human mouth is too small to accommodate wisdom teeth, which make their appearance in young adults between 15-25.)
What does “impacted” mean?
When wisdom teeth don’t have room to grow or haven’t reached their final position by age 25, they are considered impacted- no place to go and no plans to expand. Third molar impaction is the most prevalent medical, developmental disorder. A complete set of healthy teeth sometimes doesn’t leave much room for wisdom teeth to erupt.
What kind of problems can impact third molars cause?
Partially erupted wisdom teeth are breeding grounds for bacteria and germs and may lead to infection. In addition to jaw pain and gum disease, which may also develop, impacted third molars are mature sites for the growth of tumors and cysts. Not all wisdom teeth cause problems, however.
Can’t I use an antibiotic?
Antibiotics only soothe infected wisdom teeth for a short time. Since people frequently use a wide variety of antibiotics, the infection may be resistant to such medication and doesn’t solve the real problem: The tooth can’t fit in your mouth.
When is removal necessary?
It isn’t wise to wait until wisdom teeth bother you. As advised by your dentist, early removal is generally recommended to avoid problems, such as an impacted tooth that destroys the second molar. People younger than 16 heal easier too. At an early age, people should be evaluated by their dentist, who can track third molar development with the help of X-rays. Second, molars should be visible to lessen damaging them during surgery. This occurs at age 11 or 12, so wisdom teeth should be removed when the decision has been made that they cannot erupt into a good position.
What if I don’t have any symptoms?
People with symptoms of impaction, such as pain, swelling, and infection, should have their wisdom teeth removed immediately. However, those with no symptoms can avoid the chance of ever suffering from the pain of impacted wisdom teeth or achieve better orthodontic treatment results by having them removed. Symptomatic impacted wisdom teeth also should be removed to reduce the chance of unexplained pain, accommodate prosthetic appliances, or avoid cavities, periodontal disease, bone shrinkage, and tumor development.
How is the tooth removed?
Surgery for impacted wisdom teeth involves:
What is tooth extraction cost?
If you are searching for affordable tooth extraction near me than visiting Smile Ora Dental is the best choice.
MONDAY 9 AM – 5.30 PM
TUESDAY 9 AM – 5.30 PM
WEDNESDAY 9 AM – 5.30 PM
THURSDAY 10.30 AM – 6.30 PM
FRIDAY 9 AM – 3.30 PM
SATURDAY CLOSED
SUNDAY CLOSED

MONDAY 9 AM – 5.30 PM
TUESDAY 9 AM – 5.30 PM
WEDNESDAY 9 AM – 5.30 PM
THURSDAY 10.30 AM – 7 PM
FRIDAY 9 AM – 5.30 PM
SATURDAY CLOSED
SUNDAY CLOSED

MONDAY 9 AM – 5.30 PM
TUESDAY 9 AM – 5.30 PM
WEDNESDAY 9 AM – 5.30 PM
THURSDAY 10.30 AM – 7 PM
FRIDAY 9 AM – 5.30 PM
SATURDAY CLOSED
SUNDAY CLOSED
